GP Connect Clinical Feature by Dr Gill Cowen MBBS (distinction) MA(Oxon) DRCOG, DSH, FRACGP, MSportMed
Over the last few years, concussion has been increasingly topical in the lay press, with the focus on sports-related concussion and chronic traumatic encephalopathy (CTE) risk.
Despite this, only approximately 20% of concussion is sports-related. The majority of concussions result from a direct blow to the head, or transmitted force from the body, from falls, road traffic incidents and physical assault including intimate partner violence. Uncertainty relating to long term outcomes calls for optimisation of initial management of concussion injury with the aim of reducing the risk of symptom prolongation.
Concussion assessment can be difficult due to the constellation of symptoms with which patients can present, including cognitive, mood related, migrainoid, sleep related, vestibular-ocular and autonomic symptomatology, as well as the potential for evolving symptoms. It is recommended that anyone who has sustained a potential concussion seeks medical assessment for diagnostic confirmation in the company of a responsible adult.
Such assessment includes:
- Exclusion of red flags
- A history of the episode (ideally with history from an observer) and post-episode symptomatology
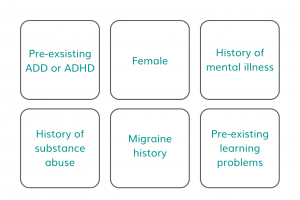
- Identification of previous traumatic brain injuries including previous concussion and confounding factors which may suggest an increased risk of delayed recovery
- Pre-injury level of function.
Other injuries may occur alongside a concussion due to the nature of the injury and must also be identified to ensure a holistic approach to management.
Confounding factors:
Further assessment includes general examination including heart rate variability, lying and standing blood pressure, cervical spine assessment, assessment for focal neurology, brief vestibular-ocular motor screening and assessment of gait and balance. A post-concussion symptom scale is also useful to assist with longitudinal symptom monitoring and in identification of those who have symptoms that fail to resolve within the typical expected recovery periods of 14 days in adults and four weeks in children and adolescents.
Initial management includes discussing expectation of symptoms and outcome. Symptom normalisation and reassurance to the patient or carer that the majority or people who sustain a concussion make an uneventful recovery is crucial part of management. A brief period of reduced physical and cognitive activity (24-48 hours), including minimisation of screen time, good sleep hygiene, alcohol avoidance and use of simple analgesia if required, should be followed with a graded and paced return to activities. This includes gentle challenging of sensitivities to noise, light and movement, and a stepwise return to cognitive and physical activities of daily living.
Involvement of school or workplace to plan a supported graduated return to learning or work program is recommended. Regular GP support beyond initial assessment for symptom monitoring, advice relating to return to work/school, driving, sport and other activities of daily living is crucial to good outcomes.
The newly developed WA “Mild Traumatic Brain Injury (Concussion)” HealthPathway provides further information relating to assessment and management of this condition.
It is hoped that with consistency of management and optimisation of care in patients who have sustained a concussion both short term and long-term outcomes for such patients can be optimised.
WA Primary Health alliance invites Interested GPs to attend the upcoming webinar Tuesday 6 September 2022.
